Patella Dislocation
What is the Patella?
The Knee Patella or Kneecap is a protective bone attached to the quadriceps muscles of the thigh by quadriceps tendon.
The Patella attaches with the femur bone and forms a patellofemoral joint. The Patella is protected by a ligament which secures the kneecap from gliding out and is called the medial patellofemoral ligament (MPFL).
What is Patellar Dislocation?
Dislocation of the patella occurs when the patella moves out of the patellofemoral groove, (called the trochlea) onto a bony head of the femur.
If the kneecap partially comes out of the groove, it is called a subluxation and if the kneecap completely comes out, it is called a dislocation.
Patella dislocation is commonly observed in young athletes between 15 and 20 years and commonly affects women because the wider pelvis creates lateral pull on the patella.
Causes of Patella Dislocation
Some of the causes for patella dislocation include
- A direct blow or
- Trauma,
- Twisting of the knee while changing the direction,
- Muscle contraction, and
- Congenital defects. or
- When the MPFL is torn.
What are the Symptoms of Patella Dislocation?
Many patients report a “pop” in their knee after a twisting injury or a direct blow to the knee. Some patients visualise the kneecap sitting on the outer surface of the knee.
The kneecap often “pops” back in when the knee straightens. Sometimes the patient requires a visit to the Emergency Department to put it back in place usually under sedation.
The experience is usually associated with severe pain until the kneecap is back in place. There is commonly gross swelling in the knee, which together with pain impairs the range of movement in the knee. Most patients require the initial use of crutches, a knee brace and analgesia.
Subluxation tends to be much less painful, associated with less swelling and often does not require hospitalisation.
The common symptoms include
- pain,
- tenderness,
- swelling around the knee joint,
- restricted movement of the knee,
- numbness below the knee, and
- discolouration of the area where the injury has occurred.
What is the Difference Between Dislocation and Subluxation?
Dislocation is when the patella completely dislodged from its normal position in the knee and lies on the outside of the thigh. Sometimes the patella can spontaneously go back into place (reduce) and other times a manual reduction is required by either the patient or a healthcare worker.
Subluxation is when the patella goes partly out of place. It is often referred to as a “partial dislocation”. Generally, this occurs very quickly and is much less painful.
Both dislocation and subluxation are spectrums of the condition referred to as patella instability.
How Does a Patella Dislocate?
Usually, it occurs with a non-contact twisting injury as the knee is bending.
Less commonly it occurs with a direct blow to the inner side of the patella, which knocks it out of place.
What are the Risk Factors for Patella Instability?
There are several well-recognised risk factors for patella instability. These include
- Female gender. Much more common when compared to males
- “Loose” joints. Some patients, more often female, have generalised laxity
- Abnormal shape of the front of the thigh bone (femur) in which the kneecap usually sits. Known as the trochlear.
- Patients with a high kneecap. Known as patella Alta.
- Abnormal alignment of the knee. Also known as “knock-kneed” where the knee points inward (valgus alignment).
- Abnormal rotation of the hip or thigh bone
What Should I do after an Episode of Knee Instability?
Initial treatment aims to control pain and swelling through a combination of rest, ice, compression and elevation (RICE). This is usually supplemented with simple analgesia such as a non-steroidal anti-inflammatory medication.
If the knee has been placed into a splint, it is important to remove the splint as swelling and pain allow, to undergo gentle knee movement as this will minimise the amount of muscle wasting that will invariably occur.
If you have been given crutches, provided x-rays have been taken to ensure you don’t have any fractures, you should try and take some weight through the leg, as pain will allow. This will also lessen the muscle wasting as well as bone deconditioning (disuse osteopenia) that will occur.
Treatment of Patellar Dislocation/Patellofemoral Dislocation
Your doctor will examine your knee and suggest diagnostic tests to confirm the condition and provide treatment. These diagnostics could include:
- X-ray,
- CT scan, and
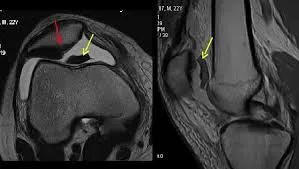
- MRI scan
Non-Surgical Treatments
Conservative non-surgical treatment includes:
- PRICE (protection, rest, ice, compression, and elevation)
- Non-steroidal anti-inflammatory drugs and analgesics to treat pain and swelling
- Braces or taping.
- Footwear to control gait while walking or running and decreases the pressure on the kneecap.
- Physiotherapy is recommended which helps to control pain and swelling, prevent the formation of scar tissue.
A physiotherapist will extend your knee and apply direct lateral to medial pressure to the knee which helps in relocation. It includes straightening and strengthening exercises of the hip muscles and other exercises which will improve range of motion.
Do I need to see an Orthopaedic Surgeon?
You should see a surgeon for a thorough assessment, investigation and treatment plan.
You may require an MRI scan. In a small percentage of cases, the dislocation process causes a fragment of cartilage to be dislodged.
This fragment, depending on its size, may be able to be pinned back in place or could be removed via keyhole surgery to prevent it behaving like a loose body and jamming in your knee.
The MRI scan also allows risk factors to be determined which may influence your likelihood of future dislocations.
What are the chances of having another episode of instability?
Most patella dislocations will occur only once. The risk of another dislocation after one dislocation is about 15%, this rises to over 50% after a second dislocation. The risk is lower in males and those with a direct blow that caused the dislocation.
Who should have surgery?
In a minority of patients, recurrent instability occurs. This can vary from the patella completely dislocating again to episodes where the patella feels like it will “pop-out” without actually occurring (patella apprehension or subluxation).
These patients may benefit from surgical intervention.
Surgical Treatment for Patellofemoral Dislocation
This depends on many factors including
- The age of the patient
- Any underlying mechanical abnormalities that predispose to instability
- Recurrent patella dislocation
The two most common procedures that Dr Ferguson would recommend would be MPFL reconstruction +/- (dependant on the results of scans) tibial tubercle transfer:
- Medial patellofemoral ligament (MPFL) reconstruction: In this procedure, the torn MPF ligament is reconstructed using a grafting technique. Grafts are either harvested from the hamstring tendons, located at the back of the knee, or an artificial ligament used and are fixed to the patella and femur using screws. This procedure is also performed using an arthroscope.
- Tibial tubercle transfer: Tibial tubercle is the bony attachment of the patella tendon on the tibia. In this procedure, the tibial tubercle is moved down or towards the centre which is then held by two screws. The screws hold the bone in place and allow faster healing and prevent the patella from sliding out of the groove. This procedure is also performed with the aid of an arthroscope.
After the surgery, Dr Ferguson will suggest you use crutches for a few weeks, prescribe medications to control pain and swelling, and recommend physiotherapy which will help you to return to your sports activities at the earliest. If you have a tibial tubercle transfer then you will be in a knee brace.