Total Hip Replacement
What is a Total Hip Replacement?
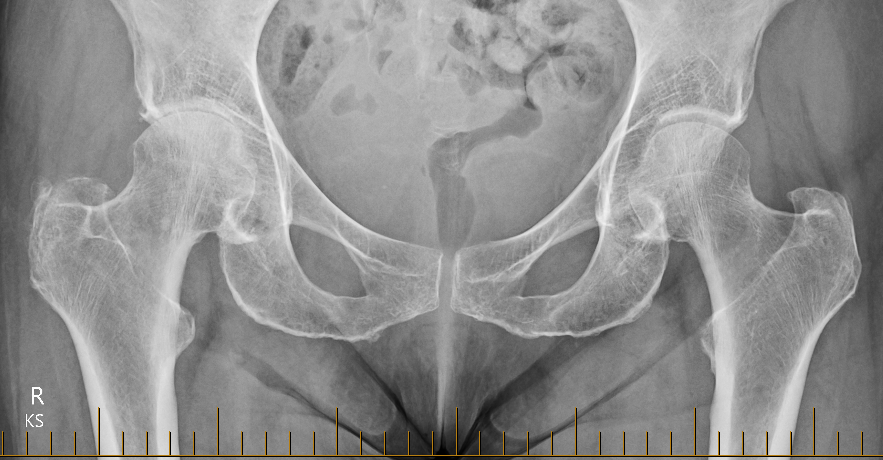
A total hip replacement (total hip arthroplasty) is a quality of life operation. It involves replacing the worn ball and socket of the hip with metal, ceramic and plastic (highly cross-linked polyethylene) components.
A hip replacement is one of the most successful operations that any orthopaedic surgeon does, and once done should last for decades (90% are still functioning after 20 years).
Who is a candidate for Total Hip Replacement Surgery?
Adults, usually over the age of 50, with a degenerate hip causing all or some of:
- Pain
- Stiffness
- Reduced mobility
These symptoms would usually have been present for many months or even years, often getting worse over time. Non-operative measures should have been tried, including weight loss, activity modification, regular analgesia. Once these are no longer enough, and the hip is having a significant impact on your quality of life, then a total hip replacement can be considered.
What is involved?
Once the decision has been made to proceed with surgery, Dr Ferguson will explain the procedure and the risks (see below). A date for surgery is usually planned but can be deferred. A booking form will be completed and you will be asked to sign a consent form. These forms are then taken to the Armidale Private Hospital where the administration staff will process the paperwork and check health fund details and eligibility. They will arrange for you to come to the pre-anaesthetic clinic (PAC) to see the anaesthetist and nurse, usually a couple of weeks prior to surgery.
Dr Ferguson will also give you a referral for a CT scan which you can take to i-Med Radiology (or Inverell Diagnostic Radiology) to get a scan that is used for the Mako SmartRobotics 3D planning. This scan should be done at least 2 weeks prior to surgery.
The operation itself is usually done under a spinal anaesthetic with sedation. The procedure usually takes about 60-90 mins. After spending some time in recovery you will then be transferred back to your room on the ward. The physiotherapist will visit you later in the day to get you to stand and to take some steps.
As the local anaesthetic wears off, the pain will increase. You will be prescribed both long-acting and short-acting narcotic pain killers to control this. On the day after surgery, you will have a routine blood test and an x-ray. Dr Ferguson will show you the x-rays to help explain what he has done. The physiotherapist will visit twice a day to show you exercises to help with your walking. Initially, you will be walking with a frame, but usually, progress to a single walking stick by discharge.
Discharge home is usually on day 3.
Who is a candidate for Total Hip Replacement Surgery?
Adults, usually over the age of 50, with a degenerate hip causing all or some of:
- Pain
- Stiffness
- Reduced mobility
These symptoms would usually have been present for many months or even years, often getting worse over time. Non-operative measures should have been tried, including weight loss, activity modification, regular analgesia. Once these are no longer enough, and the hip is having a significant impact on your quality of life, then a total hip replacement can be considered.
What is involved?
Once the decision has been made to proceed with surgery, Dr Ferguson will explain the procedure and the risks (see below). A date for surgery is usually planned but can be deferred. A booking form will be completed and you will be asked to sign a consent form. These forms are then taken to the Armidale Private Hospital where the administration staff will process the paperwork and check health fund details and eligibility. They will arrange for you to come to the pre-anaesthetic clinic (PAC) to see the anaesthetist and nurse, usually a couple of weeks prior to surgery.
Dr Ferguson will also give you a referral for a CT scan which you can take to i-Med Radiology (or Inverell Diagnostic Radiology) to get a scan that is used for the Mako SmartRobotics 3D planning. This scan should be done at least 2 weeks prior to surgery.
The operation itself is usually done under a spinal anaesthetic with sedation. The procedure usually takes about 60-90 mins. After spending some time in recovery you will then be transferred back to your room on the ward. The physiotherapist will visit you later in the day to get you to stand and to take some steps.
As the local anaesthetic wears off, the pain will increase. You will be prescribed both long-acting and short-acting narcotic pain killers to control this. On the day after surgery, you will have a routine blood test and an x-ray. Dr Ferguson will show you the x-rays to help explain what he has done. The physiotherapist will visit twice a day to show you exercises to help with your walking. Initially, you will be walking with a frame, but usually, progress to a single walking stick by discharge.
Discharge home is usually on day 3.
Surgical Approach
The way a surgeon cuts the soft tissues to get down to the hip is called the surgical approach. Two of the most common approaches are the “Posterior Approach” and the “Direct Anterior Approach”. Dr Ferguson has been trained in the use of both approaches.
Posterior Approach
- The most commonly used approach
- Involves patient being placed on their side with the surgical side up
- Skin incision (usually 10-15cm long) is on side of the hip
- The gluteus maximus (the big muscle making up your bottom cheek) is split, in line with its fibres, and some small tendons (short external rotator tendons, Dr Ferguson preserves the Piriformis tendon) and the capsule at the back of the hip are released. These are reattached with sutures through the bone later.
Direct Anterior Approach
- The patient is lying flat on the operating table
- Skin incision (usually 10-15cm long) is on front of the hip
- Space is developed between two of the thigh muscles (tensor fascia lata and Sartorius) and then a cut is made in the capsule at the front. Often some tendons are released (which could include short external rotators, piriformis, rectus femoris), but these are not usually reattached.
Through a combination of personal experience, performing both approaches, and reviewing the current research evidence (for those inclined to review themselves, links to some high-quality research are provided below), it is Dr Ferguson’s opinion that the only significant consistent difference between the two approaches is the position of the scar!
A well-done hip replacement is a fantastic operation, in terms of pain relief and improved quality of life, regardless of which approach is used.
- Association Between Surgical Approach and Major Surgical Complications in Patients Undergoing Total Hip Arthroplasty https://pubmed.ncbi.nlm.nih.gov/32181847/
- Clinical, functional and radiographic outcomes of primary total hip arthroplasty between direct anterior approach and posterior approach: a systematic review and meta-analysis https://pubmed.ncbi.nlm.nih.gov/32487060/
- Patient-Reported Outcomes Following Total Hip Arthroplasty: A Multicenter Comparison Based on Surgical Approaches https://pubmed.ncbi.nlm.nih.gov/31926776/
What are the risks of the operation?
All operations have risks, and hip replacements are no exception. Dr Ferguson will outline these to you before you sign the consent form. They include:
- Pain
- Bleeding
- Infection
- Damage to nerves or blood vessels
- Blood clots (leg/lungs)
- Dislocation
- Fracture
- Limb length discrepancy
- Loosening
Apart from pain, most patients don’t have any of these problems. The risk of a complication is about 5 in 100. The risk of a serious complication, such as deep infection, is less than 1 in 100.
Although the risk of dislocation is low, Dr Ferguson advises you to adhere to the following advice for the first 6 weeks after surgery:
- Keeps your legs apart and feet facing forwards
- Do not bend at the waist beyond a right angle
- Do not twist at the waist or cross your legs